TMD and Its Connection to Migraine
November is TMJ Awareness Month. This month is dedicated to educating the public about temporomandibular joint disorders (TMD), which affect the jaw joint, muscles and related structures.
What is TMJ?
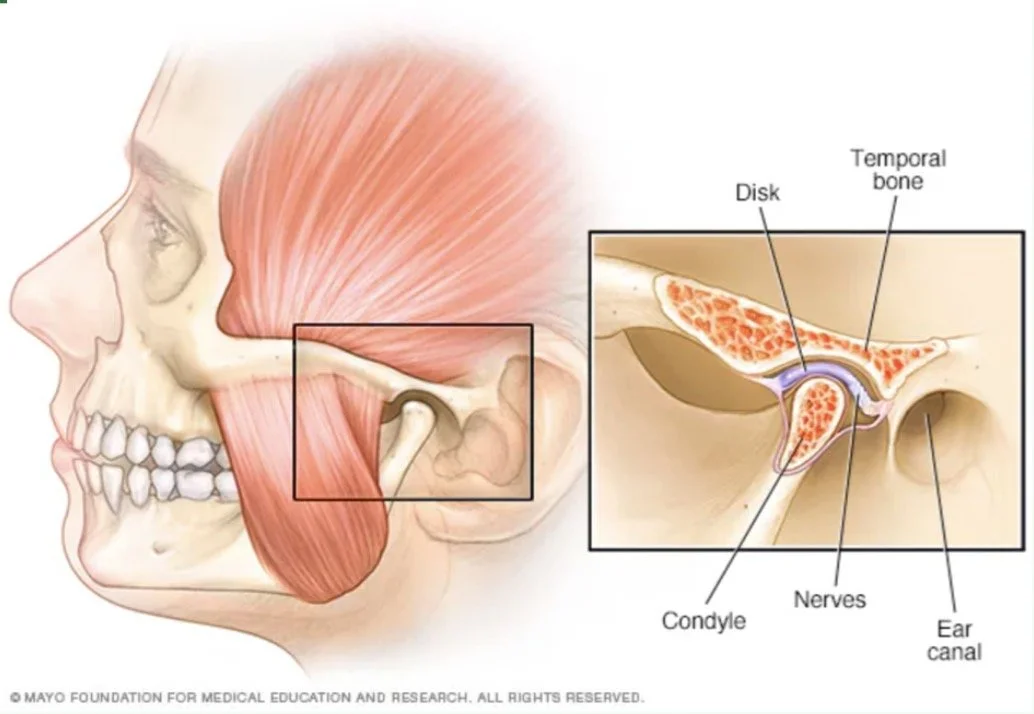
The temporomandibular joint connects your jawbone to your skull and allows you to chew, speak, and yawn.
What is TMD?
Temporomandibular joint disorder (TMD) is a group of conditions characterized by pain and dysfunction involving the temporomandibular joint (TMJ), the chewing muscles, and associated head and neck structures.
TMD Symptoms:
Jaw pain
Limited or asymmetric jaw movement
Clicking, popping, or grating sounds when moving your jaw
Locking of the jaw
Headaches
Ear discomfort
Difficulty chewing
How does TMD connect to migraine?
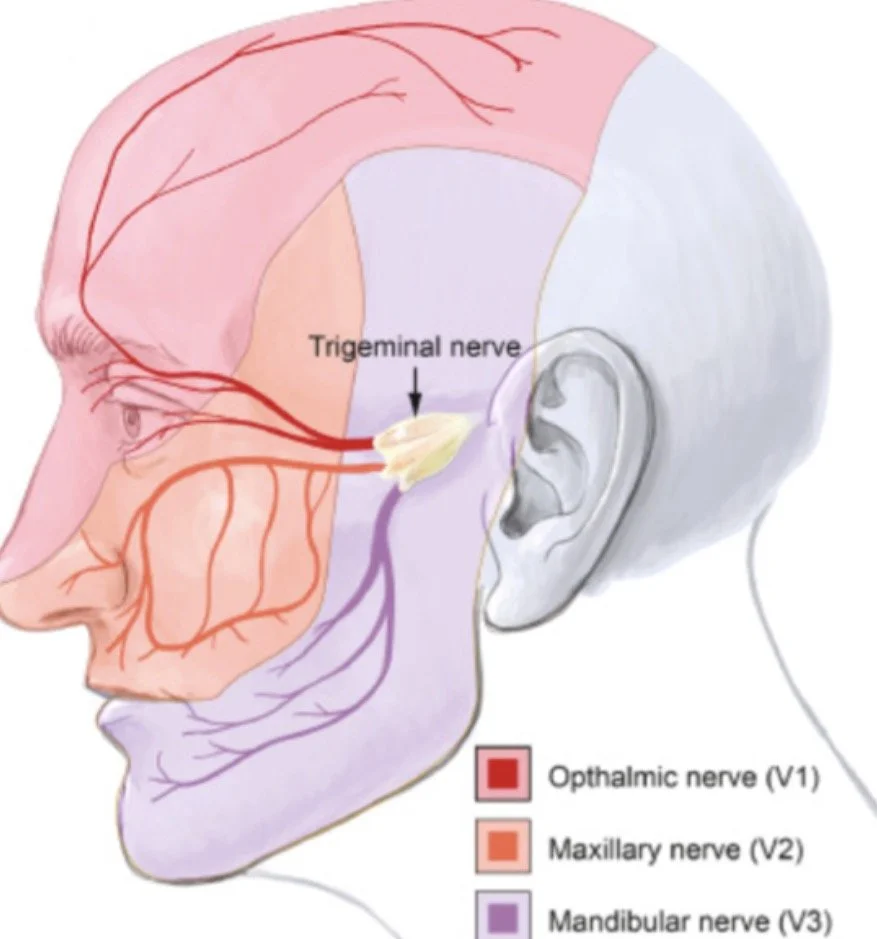
Pain in the jaw significantly increases the odds of migraine occurrence [1-2]. TMD can contribute to migraines through shared nerves and muscles, especially the trigeminal nerve. The trigeminal nerve provides feeling to the face, front of the scalp, nose, mouth, and teeth, and it also controls the muscles used for chewing. When the jaw joint or the muscles used for chewing are inflamed or not working properly, they can stimulate the trigeminal nerve that can trigger headaches or migraines [3-5]. Inflammation of the jaw can release a chemical called calcitonin gene-related peptide (CGRP) in trigeminal pathways that can lead to migraines [4]. Teeth grinding and clenching can also exacerbate TMD and migraines.[3] Treating TMD may help decrease the frequency and severity of headaches and migraines
Treatment:
Multidisciplinary management is recommended for patients with both TMD and migraine, involving collaboration between headache medicine, dentistry and physical therapy.[3] The goals of treatment for TMD are to decrease pain and to improve function. Physical therapy can help reduce joint inflammation, improve joint mobility, and reduce muscle pain.
Are you ready to figure out if your jaw pain is contributing to your migraines? Schedule your free phone consult below!
References:
1. Association Between Primary Headaches and Temporomandibular Disorders: A Systematic Review and Meta-Analysis. Réus JC, Polmann H, Souza BDM, et al. Journal of the American Dental Association (1939). 2022;153(2):120-131.e6. doi:10.1016/j.adaj.2021.07.021.
2. Painful Temporomandibular Disorder Is Associated With Migraine in Adolescents: A Case-Control Study. Fernandes G, Arruda MA, Bigal ME, Camparis CM, Gonçalves DAG. The Journal of Pain. 2019;20(10):1155-1163. doi:10.1016/j.jpain.2019.03.010.
3. Optimising Combined Treatment for Migraine and Temporomandibular Disorders (TMDs).
Romero-Reyes M, Akerman S, Rapoport AM. Cephalalgia : An International Journal of Headache. 2025;45(9):3331024251368882. doi:10.1177/03331024251368882. New Research
4. Interplay of Oral, Mandibular, and Facial Disorders and Migraine.Teruel A, Romero-Reyes M. Current Pain and Headache Reports. 2022;26(7):517-523. doi:10.1007/s11916-022-01054-6.
5. An Update on Temporomandibular Disorders (TMDs) and Headache.
Romero-Reyes M, Klasser G, Akerman S. Current Neurology and Neuroscience Reports. 2023;23(10):561-570. doi:10.1007/s11910-023-01291-1.
Image References
1. Mayo Clinic Staff. TMJ disorders — Symptoms & causes. Mayo Clinic. Updated December 24, 2024. Accessed November 16, 2025. https://www.mayoclinic.org/diseases-conditions/tmj/symptoms-causes/syc-20350941
2. Trigeminal Neuralgia. Ferneini, Elie M. Journal of Oral and Maxillofacial Surgery, Volume 79, Issue 11, 2370 - 2371